
Cervical osteochondrosis is a progressive degenerative dystrophic lesion of the intervertebral discs located between the first 7 vertebrae. Vertebrae 1 to 7 belong to the cervical spine.
Pathological changes against the background of osteochondrosis lead to deformation of the vertebrae, which ultimately disrupts the blood supply, nerve conduction in the neck and areas of innervation of damaged nerves.
Osteochondrosis of the cervical spine can be an independent disease or combined with osteochondrosis of other parts - thoracic and lumbar.
Main symptoms
The main symptom of cervical osteochondrosis is pain, the location and nature of which depend on the location of the injury. Most often, it is felt in the neck area, on one or both arms.
This disease is characterized by unilateral pain, which can hurt any part of the arm - shoulder, forearm, hand and even fingers. Many patients complain of headaches and dizziness.
The pain syndrome can also be felt in the chest, supraclavicular region or spread across the back. For some, the pain is concentrated at the base of the neck or throat.
Osteochondrosis of the cervical spine is characterized by a variety of symptoms and is often accompanied by a tactile sensitivity disorder, muscle weakness, decreased visual and auditory acuity, tachycardia and panic attacks.
Attention!
Sometimes osteochondrosis is complicated by vertebral artery syndrome, which may require emergency hospitalization of the patient.
First signs
In the initial stages, the manifestations of osteochondrosis are more reminiscent of ordinary fatigue after a busy day and occur periodically. At night, discomfort and pain appear in the neck, heaviness and pain in the head, especially in the occipital region. Possible clicks and creaks when turning the head.
Signs of cervical osteochondrosis in women are more pronounced than in men and are often accompanied by an unstable psycho-emotional state. In addition, men suffer from this disease much less often.
Exacerbation of chondrosis often occurs during menopause, when hormonal changes occur in the female body and the immune system weakens. Certain difficulties arise in diagnosis due to signs similar to those of many other diseases.
Men react less to little things, like a tightness in the neck, and often simply don't notice suspicious symptoms. In addition, the symptoms of cervical osteochondrosis in men may not appear for a long time, which is explained by the peculiarities of the anatomy.
Men naturally have more developed and stronger muscles, which creates additional support for the spine. The muscular structure serves as a kind of armor that protects the vertebrae and prevents their deformation.
Vertebral artery syndrome (VAS)
The clinical picture of SPA is usually represented by several symptoms, but only one of the possible ones can be observed:
- headache with predominant localization in the back of the head and base of the skull - basilar migraine, accompanied by classic symptoms: loss of coordination, nausea leading to vomiting, tinnitus, less often - speech impairment;
- dizziness that occurs when turning the head. They may be accompanied by vomiting, darkening of the eyes and difficulty coordinating movements;
- eye fatigue due to stress, flickering spots and bright flashes before the eyes, and in some places, loss of visual fields. Patients may complain of pain, redness and a feeling of sand in the eyeball, inflammation of the conjunctiva;
- constant or episodic tinnitus, the nature of which varies depending on the position of the neck. There may be mild deafness, ear congestion, and lack of response to a low voice. In some cases, paracusis was observed - selective audibility of sounds, in which a person hears better in the presence of extraneous noise than in complete silence;
- vegetative symptoms always occur when osteochondrosis worsens and are most often combined with other symptoms. These may be hot flashes or chills, increased sweating, cold feet and hands, a feeling of shortness of breath, increased blood pressure and poor sleep;
- TIA - transient ischemic attacks - accompany mechanical clamping of the vertebral artery and are manifested by double vision, temporary partial blindness with loss of visual fields, dizziness with vomiting, speech and swallowing function disorders;
- Fainting can be a consequence of sudden turns of the head or its uncomfortable position. Loss of consciousness lasts for varying periods of time and leaves weakness in the limbs;
- Drop attacks are sudden falls, usually without loss of consciousness, caused by a sudden rush of blood to the brain when the head is thrown back. The immediate cause is paralysis of the legs, but motor function is quickly restored.
Headaches and dizziness
Most patients with cervical chondrosis experience this symptom, but it may be absent. The cause of dizziness is associated with compression of the main arteries and blood vessels, which disrupts the transport of oxygen to the nervous tissue of the medulla oblongata and spinal cord.
Under the influence of mechanical trauma to the vertebral structures and chronic ischemia of nerve fibers, increased sensitivity and irritation of nerve endings occur, which ultimately causes cervical dizziness.
Dizziness can be accompanied by uncertainty of movement, increased heart rate, spikes in blood pressure and increased sweating in the face and shoulder area.
Headache is a frequent companion of cervical chondrosis. It is paroxysmal in nature, the duration of the attack varies from several hours to several days. The intensity of the pain varies, but appears with enviable regularity.
The headache is caused by compression of the vertebral artery due to changes in the position of the vertebrae and discs. Due to compression of the vessel, the blood supply to the brain is disrupted, which causes pain.
Reference:
The cause of pain can also be muscle spasm, typical of osteochondrosis.
Panic attacks
Panic attacks are also associated with reduced brain nutrition and cause the following symptoms:
- fever attacks or chills, increase in body temperature;
- numbness, tingling in the limbs, muscle cramps, impaired motor capacity;
- dizziness, loss of coordination, darkening of the eyes;
- pain behind the sternum or in the chest on the left, rapid pulse, increased blood pressure;
- insomnia, fear of death or mental confusion, confusion;
- shortness of breath, difficulty breathing until suffocation, lump in the throat;
- abdominal discomfort and pain, indigestion, frequent urination.
Sore throat
The throat with osteochondrosis hurts, as a rule, when the 4th cervical vertebra is damaged or displaced. The location is usually unilateral, as the vertebrae and discs shift to one side.
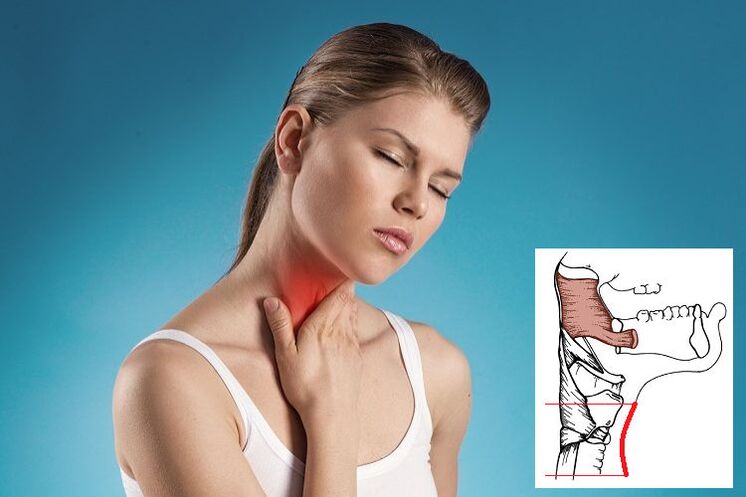
Due to pinching of the roots, spasms and tension of the pharyngeal muscles occur, accompanied by pain. The throat feels heavy and full and it becomes difficult to breathe. However, there are no mechanical obstacles to free breathing and swallowing, there are no foreign objects or tumors in the esophagus and larynx.
It is typical that medications for tonsillitis or sore throat, rinsing and inhalation have no effect.
The source of the pain is in the area between the thyroid cartilage and the jugular cavity. The nature of the pain varies from mild to debilitating.
Treatment
Complex treatment of cervical osteochondrosis includes several methods - taking medications, doing therapeutic exercises, attending physiotherapy sessions and massages. If you wish, you can use folk remedies and make various compresses, prepare infusions and decoctions.
If the disease worsens, bed rest is recommended. In addition, you should lie on a flat, rather hard and elastic surface - a sagging sofa or feather bed will not work.
Attention!
Severe pain requires immediate medical attention.
To correct the cervical spine, your doctor may prescribe the use of a Shants collar. Supports the neck in an anatomically correct position, eliminating movements and, therefore, pain.
Medicines are selected taking into account existing symptoms and diagnostic results. If hernias and protrusions are detected, treatment may be surgical.
| Drugs | Action |
|---|---|
| Vasodilators and nootropics | Improves cerebral circulation, dilates blood vessels, relaxes smooth muscles, reduces the frequency of nerve signals |
| Preparations with chondroitin and glucosamine | Restoration of the cartilaginous tissue of the discs, delaying degenerative processes |
| Muscle relaxants | Relieving muscle spasms |
| Nonsteroidal anti-inflammatory drugs | Relief of the inflammatory process, tissue swelling |
| Painkillers | Pain elimination |
| Opioids | For severe pain that cannot be relieved by conventional means |
| Vitamin complexes containing vitamins B, A, C, calcium | Strengthening nervous, muscle and bone tissue, general healing effect |
| Antidepressants and sedatives | Dealing with the stress caused by constant pain |
Home treatment
It is not recommended to lie at home for a long time and follow bed rest, and after the acute symptoms disappear, you need to switch to active actions. You should start with simple exercises and gradually move to more intense exercises.
- Exercise 1 – self-extension. Standing, with your arms lowered along your body, tilt your head to the right and, at the same time, extend your left hand. Stay in this position and repeat the exercise on the other side.
- Exercise 2 – self-massage. Place the towel over your shoulders and, holding the ends, pull them in one direction or another.
- Exercise 3 – turn your head left and right, tilting to the right and then to the left shoulder.
- Exercise 4 – same with hand counteraction: when turning or tilting, press into the temple, creating additional resistance.
Tips to prevent osteochondrosis
Tip #1
Physical education is the main way to combat the aging of the body and the development of intervertebral disc dystrophy. Typically, daily exercise and visiting the pool at least once a week are sufficient. All this allows you to strengthen the muscular corset of the spine.
Tip #2
Even a healthy person needs massage sessions, it is recommended to carry them out annually.
Tip #3
It is very important to monitor your weight and avoid gaining extra pounds.
Tip #4
When working for a long time in a forced position, it is necessary to take breaks, change body position and warm up.
Tip #5
Eating well means consuming enough vitamins and microelements with food.
Tip #6
Try not to lift or carry heavy objects and, if necessary, wear a supportive corset.
Common questions
When do you need to see a doctor urgently?
The reasons for immediate consultation and even an ambulance call are:
- persistent numbness in the arms or legs;
- intense pain that is not relieved by conventional painkillers;
- movement disorder;
- severe headache, dizziness, loss of coordination and other signs of a stroke;
- "locking" of the back in a certain position, drastically limiting movement.
Is it possible to cure chondrosis forever?
No, this is a chronic disease with periodic exacerbations. Even after treatment and following all the doctor's recommendations, the cartilage in the affected area of the disc is replaced by scar tissue. In other words, the structure of the segment has already been damaged and this process is irreversible. However, with some effort on the part of the patient, a high quality of life can be achieved.



















